The Missouri Division of Developmental Disabilities was established in 1974 to support the unique needs of individuals, family members and caregivers who experience a developmental disability (DD). The Division understands that individuals and those who support them, have diverse strengths, abilities, needs and challenges.
Individuals and families identify that they face greater challenges in their attempt to navigate day-to-day life. They state the need for:
- Relevant Information;
- Resources;
- Access to valuable supports and services, as well as;
- The opportunity to share their life experiences with others in similar situations to ensure long term success.
The services and supports provided by the Division are centered on empowering individuals and families to:
- Experience quality and meaningful lives;
- Become valued members of their communities where they:
- Live
- Work
- Play
- Learn
- And pursue their life goals.
- What is a developmental disability?
A developmental disability is:
- A disability which is attributable to an intellectual disability, cerebral palsy, epilepsy, head injury, autism, or a learning disability related to brain dysfunction, or any other mental or physical impairment;
- Occurs prior to the age of 22;
- The disabling condition is likely to continue indefinitely;
- Results in Substantial Functional Limitations in 2 of the six areas listed below:
- Self-Care
- Receptive/ Expressive Language
- Learning
- Mobility
- Self-Direction
- Capacity for Independent Living/ Economic Self-Sufficiency;
- Requires some level of habilitative training. Habilitative means skill development that assists the individual learning to become more independent.
- How do I access Division of DD Services
Accessing DD services begins by contacting the local Regional Office/ Satellite Office for the County you reside in. Connect to the state map to locate your local office.
Application Process
- An Intake worker will conduct an initial interview either by phone or in person where they will gather basic demographic information such as: name, age, date of birth and the like. They will also gather information regarding the nature of the disability, names of those who would have information supporting the disability and the potential applicant’s current status with Medicaid.
- An application will be provided to the individual or their responsible party, either in person or by mail. The packet will consist of:
- Application for Services
- Rights Acknowledgment
- Financial Questionnaire
- Releases of Information (ROI)
- Intake staff will mark/ indicate where signatures or information is required.
- Once the application has been signed and completed, it will need to be returned to the appropriate Regional/ Satellite Office.
- The application will be reviewed to ensure that it is complete. Once the application is validated, the eligibility process will begin.
Eligibility Process
The eligibility process will look differently for each applicant but a few similarities are listed below:
- Medical/Psychological/Education records will be requested by utilizing the ROI’s included in the application packet.
- Eligibility Staff will review the records
- Various assessments may be completed by Eligibility Staff, if there is sufficient information noted in the records that were obtained.
- Most importantly, Eligibility Staff are available to answer questions as they come up.
- What types of Division services and supports are available?
Information Specialist System (I/S)
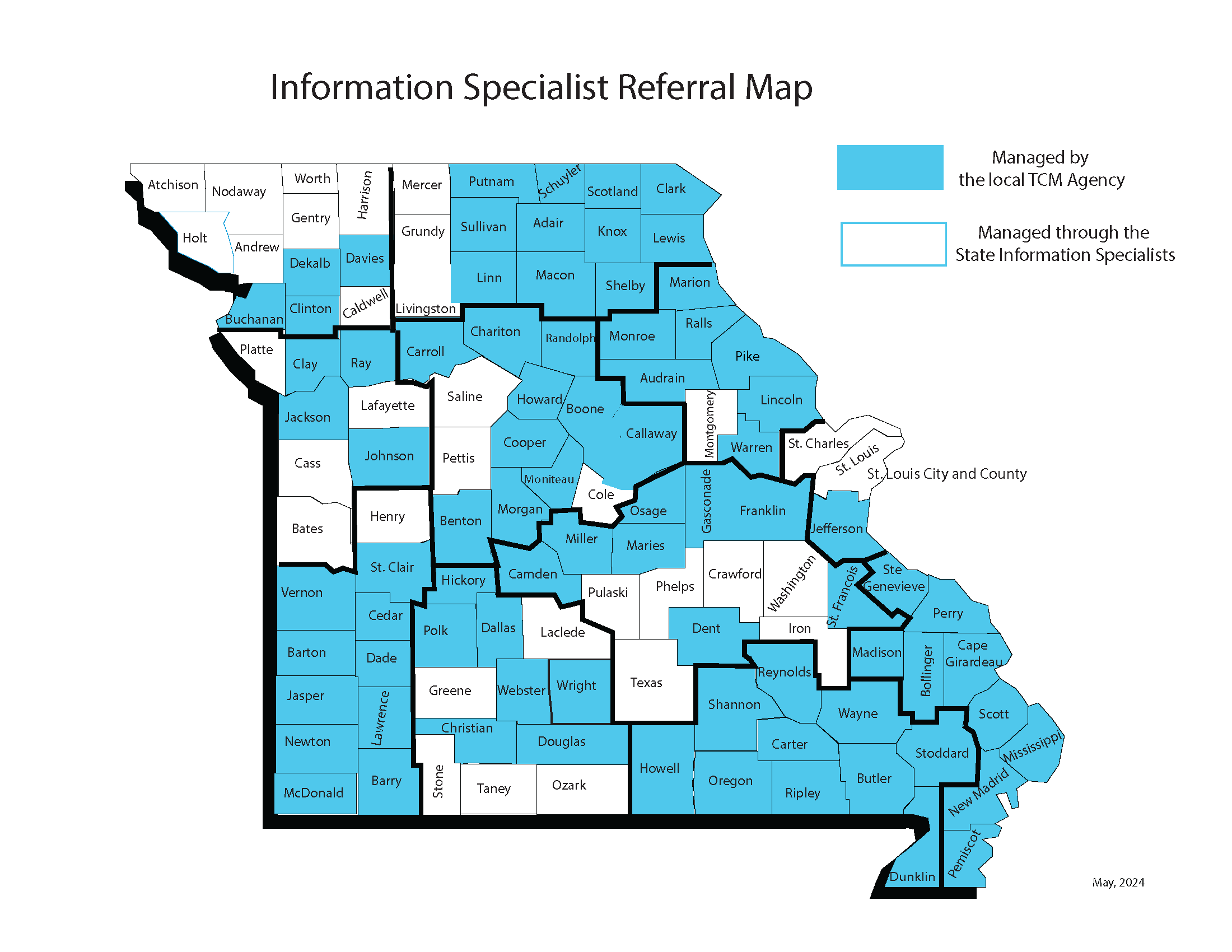
Individuals who are not currently enrolled in Medicaid and reside in the white counties will be assigned to the Information Specialist system. Information Specialist staff will work to assist the individual and or responsible party to enroll in the Medicaid system. Individuals will also receive information regarding specific topics related to the disabling condition. As the Division produces content, such as informational videos, podcasts, newsletters and the like, those will be forwarded though email as well as through social media outlets. information.specialist@dmh.mo.gov
1-800-241-2741.
Support Coordination/ Case Management
Individuals residing in the blue counties, regardless of their relationship to Medicaid System will receive support coordination services. Support Coordination means that the Division itself or a contracted Targeted Case Management provider will work with the individual/ responsible party to identify specific needs and goals and a plan will be developed to access any and all available resources to meet those goals. This can be as simple as a yearly face to face meeting, school advocacy or direction on accessing other services within the community. It can also be as involved as accessing funded services offered by the Division through various funding sources.
Purchased Services
Any support beyond Support Coordination is considered a funded direct support service. New requests for funding require that the individual in need has active Medicaid. Missouri works in partnership with the federal government to share the costs of services through participation in Medicaid Waivers. The specific requirements to access such funding can be discussed in greater detail with the assigned Support Coordinator.
There is one exception to this rule. Any individual with an Autism diagnosis has the ability to access specific funding distributed by the five Parent Advisory Councils across the state. This allotment of funding is provided solely by Missouri tax dollars and not in partnership with the Federal Government, which means participating in Medicaid is not a requirement.
- How are services approved?
Following eligibility, the individual, family or guardian meets with a Support Coordinator to develop a plan, called an Individual Support Plan (ISP). This ISP includes a description of the individual, the person’s goals and needs, what outcomes are expected to be achieved, and the particular services and funding being requested. This plan is then reviewed at the Regional or Satellite office for approval.
If the Division does not have enough funds to serve everyone who is approved for services, then a Priority of Need process determines who can begin their services and who must wait.
- What other agencies provide services and supports?
Missouri has few restrictions when it comes to accessing services and supports from other state and private agencies. Typically, if the individual qualifies for the service or support, then they can access it regardless of their relationship to other state and private agencies. *See exceptions below. A list of some agencies and services that can be accessed include:
Missouri First Steps - Administered by the Department of Elementary and Secondary Education and serves children 0-3 years old who have a qualifying medical condition or who demonstrate a Half Age Delay in development.
WIC - Administered through the Department of Health and Senior Services, the program provides supplemental food and nutrition education to pregnant women, new mothers and children up to age five. Individuals must be certified in person to receive services. WIC certification and services are offered in 117 agencies across the state, primarily at your local county health department.
Special Healthcare Needs - Administered by the Department of Health and Senior Services, providing service coordination and authorization for medically necessary services for children and medically fragile adults with special health care needs that meet medical and financial eligibility requirements.
Division of Vocational Rehabilitation - Administered by the Department of Elementary and Secondary Education, assisting individuals with various disabling conditions to find employment either through job search assistance or education/ training assistance.
Family Support Division - Administered by the Department of Social Services, providing such programs as MO HealthNet (Medicaid), SNAP, TANF, and others.
Senior and Disability Services - Administered by the Department of Health and Senior Services, providing in-home supports to adults with on-going medical and or physical needs who have active MO HealthNet.
HIPPS - (Health Insurance Premium Payment) Administered by the Department of Social Services. It exists to reimburse the cost of private health insurance premiums for those who are active with the MO HealthNet system. The reimbursement takes place if it is determined to be cost effective. Each case is reviewed on an individual basis.
*Exception to the rule:
Many state agencies have arrangements with the federal government to share the costs of certain services. These are typically referred to as Medicaid Waivers. Regulations state that a Missouri citizen can only access one Medicaid Waiver at a time. This means that if a person is actively receiving Medicaid Waiver services from one state agency, they are not eligible to access Medicaid Waiver services through another state agency.
- Additional Information
- MAAS Assessment and Scheduling—Key Points for Individuals and Families The Division of Developmental Disabilities has been working on a plan to make the assessment (tests) and eligibility processes better, including scheduling assessments (tests) like the MAAS. Because there has been a lot of information and updates shared about the MAAS and scheduling, the Division has created a plan that captures all of the important items in one document. This plan is called the Assessment Capacity Bridge Plan. It explains the temporary changes that should make a faster process to help individuals and families seeking or currently receiving services.
Assessment Capacity Bridge Plan—Key Points for Individuals and Families
Full Assessment Capacity Bridge Plan - Public Administrator Training - This training was developed to assist Public Administrators in navigating supports and services for those with intellectual/developmental disabilities.
- How and Where to Get Help
- Community Living and Accessible Housing
- Quality Assurance Unit
- Consumer Safety
- Acronyms and Abbreviations
- Eligibility Criteria for Services
- Olmstead Information
- Missouri Proclamation of Equal Rights for People with Disabilities as Members of Society
- Supporting Families Resource List
- Pre-admission Screening and Resident Review (PASSR)
Individual and Family Guides
- The EZ Readers were developed to provide individuals and families with plain language, easy-to-read information about the Division of Developmental Disabilities, resources, and supports.
- Supporting Families Through the Individual Support Plan (ISP) Process
- Dental Resource Guide: including tips on locating dental insurance
- A Guide to Understanding MoHealthNet Services
- HCBS Rule Overview for Individuals and Families
- HCBS Got Choice Brochure for Individuals and Families
Volunteer & Advocacy Opportunities
Links to Other Websites
- MAAS Assessment and Scheduling—Key Points for Individuals and Families The Division of Developmental Disabilities has been working on a plan to make the assessment (tests) and eligibility processes better, including scheduling assessments (tests) like the MAAS. Because there has been a lot of information and updates shared about the MAAS and scheduling, the Division has created a plan that captures all of the important items in one document. This plan is called the Assessment Capacity Bridge Plan. It explains the temporary changes that should make a faster process to help individuals and families seeking or currently receiving services.
